Stomach
Structure and Function
Structure
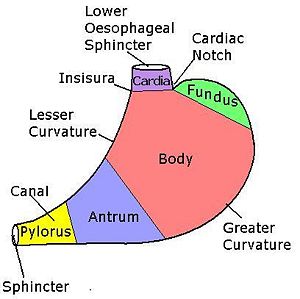
Basically a sac that can expand and shrink a bit (because of the rugae, folds in the stomach walls). It has two sphincters, the gastro-oesophageal and the pyloric (which is just made out of thickening of the circular muscle layer).
There are enzyme and HCl secreting cells, as well as mucus secreting ones.
Functions
- Storage: 1500ml capacity, collapsible and expandable (rugae)
- Formation: semifluid chyme
- Protection (HCl), kills bacteria, Mucus, prevents damage to stomach from alcohol, aspirin, NSAIDs, etc.
- Absorptive: Small amounts of H2O, alcohol, drugs
- Mechanical Digestion: muscles
- Secretive: H2O, enzymes, hormones
| Type | Location | Secretion |
|---|---|---|
| Parietal | Body + Fundus | HCl and Intrinsic Factor |
| Chief | Body + Fundus | Pepsinogen |
| Goblet Cells | Everywhere | Mucus |
| G Cells | Antrum | Gastrin |
| Enterochromaffin-like Cells | Antrum | Histamine |
| D Cells | Antrum | Somatostatin |
Arterial and Venous supply
- Left gastric: Lesser curvature
- Right Gastric: Lower part of stomach
- Right Gastroepiploic: Inferior aspect of the greater curvature
- Left Gastroepiploic: Superior aspect of the greater curvature
- Short Gastrics: Fundus
Nervous Supply
Parasympathetic:
- Left Vagus nerve applies anteriorly on the left hand side of stomach
- Right Vagus nerve applies posteriorly to the right hand side of stomach
- Functions: essentially the motor activities; secretion, digestion and muscular. It is this nerve that make the stomach churn and peristaltise food.
Sympathetic:
- Branches of the celiac plexus.????? From the sphlanchnic nerve. The only sympathetic fibres in the stomach (pain fibres)
- Functions: contains the efferent pain fibres. When stomach "drops" in fear, this nerve activates that.
Lymph
Left gastric nodes: Drain the lesser curvature and 2/3 of the body. Pancreaticosplenic, gastroepiploic and pyloric nodes: Rest of stomach.
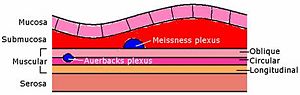
Histology
Both plexi above are parasympathetic
Clinical Conditions
Physical
Pyloric Stenosis
About: Hits mostly in first born boys at 4-6/52. It is due to hypertrophy of the pyloric sphincter.
Presentation:True projectile vomiting of milk (undigested). Child will be dehydrated, hungry and dry. You should be able to palpate an "olive".
Investigations: Test feed, ultrasound, bloods will be low in K+ and CL- (Hypochloraemic and hypokalaemic – this must be treated before surgery with IV fluids, etc)
Treatment: Cut through the pyloric sphincter muscles {+nearly +} to lumen.
Inflammatory
Chemical reflux
Alkali stuff from the duodenum is refluxed into the duodenum, as a result of stomach operation, or defective response to CCK, and/or secretin, which increase pyloric tone.
Dyspepsia
A diagnostic dead end – we don't know what's wrong, so you have dyspepsia (indigestion). Treatment with placebos is surprisingly effective (upto 60%!).
Gastropathy
Epithelial/endothelial damage without inflammation. All the usual suspects, alcohol, smoking, drugs, aspirin and other NSAIDs and H. Pylori. Can lead to ulcers and cancer. Treatment by removing the antagonist.
H. Pylori
About: Gram negative (pink) bacteria (spiral). Converts urea to NH3, causing the stomach pH > 7. Cause of both types of ulcer. HP attacks epithelial cells provoking an inflammatory response, which is ineffective against the HP. Duodenal ones are caused when a particular type of HP, just in the antrum, causes the parietal cells the make loads of HCl, which hits the duodenum with a bang.
Investigations: C13 labelled breath test
Treatment: Proton Pump Inhibitor (means less H+ is pumped out of the stomach, increasing the pH) and 2 antibiotics
Acute (NSAID induced) gastritis
NSAIDs cause exfoliation (take off the top layer) of surface epithelium. As a result mucus secretion is reduced, so the stomach is eroded (partial loss of mucosa) and develops ulcers (erosion below the muscularis mucosa). Non Steroid Anti Inflammatory Drugs can perversely cause irritation and inflammation to the stomach lining. They are commonly taken by old ladies treating their arthritis, so beware of them. They need to stop taking the NSAIDs and use a replacement, or less damaging variety.
Chronic gastritis
Autoimmune disease where antibodies attack parietal cells and intrinsic factor bindings sites which results in pernicious anaemia (gastritis with macrocytic (big red blood cell) anaemia).
Carcinoma
Cancer
Usually adenocarcinoma.
Risks: Smoking, Blood Group A, Ulcers, Long standing mucosal injury (alcohol, etc), pernicious anaemia. HP gastritis, low acid secretion. Higher risk with HP, due to high cell turnover. Diet low in fresh fruit and veg.
Presentation: Intestinal metaplasia due to cross linked lymph common, so spreads easily. Insidious onset (very slow, and late to present) so vast majority inoperable on presentation (10-15% 5 year survival). Loss of appetite and weightloss, vomiting, enlarged lymph nodes, stomach mass.
Investigations: Bloods for anaemia and electrolyte loss, gastrin levels (in case it's a hormone secreting 'un), CT, Ultrasound, Gastroscopy.
Treatment: Normally chemo and radio to try and make it operable. Because the lymphatic vessels of the mucosa and submucosa are linked across the stomach, cancer often mestatises. Because of this, it is very often treated with a total gastrectomy, which includes the bottom part of the oesophagus and first part of the duodenum. The oesophagus is left linked straight to the duodenum.
Ulceration
Peptic Ulcers
- Gastric: Old and male, gets worse with food
- Duodenal: Young and male, gets better with food and worse at night.
The antrum, where the gastrin is secreted is often the home of these. They occur in the alkaline producing mucosa, usually on, or close to the lesser curvature. The regurgitated duodenal contents/alkali from HP strip away the mucus, which exposes the epithelial cells to be attacked by acid, which creates a cumulative increase in mucosal permeability – once its started, it gets easier. Usually when mucus and epithelial cells get attacked – %color=#ff0000 %rarely from too much acid%%.
Bad stuff that can happen:
- Perforation: where the gastric contents leak into the cavity, causing peritonitis
- Penetration: Where it erodes into something else – like an organ
- Haemmorrage: Eroded blood vessels at base of ulcer, leading to blood going EVERYWHERE!